Information on this site shall be considered as holistic, alternative and spiritual advice only. For medical advice and treatment a GP, medical professional and/or Certified Hijama Therapist should be consulted. In all circumstances where lifestyle changes, supplements, or other foods are suggested your GP should be consulted. Client Safety is the number one priority.
Cupping / Hijama Points Treatment Plan for Neuritis
Allow 2-4 weeks between sessions – longer if required. Hijama Points shown for each session should ONLY be used to guide the therapist. Body size, cup size, and any other conditions need to considered and appropriate care and attention taken. The number of sessions shown can be increased or reduced depending on the condition of the client.
Complete Treatment Plan
Click here for Session 1Click here for Session 2
Click here for Session 3
Click here for Session 4
Click here for Session 5
Click here for Session 6
Standard Wet Points – 1,55,110,111,112,113,114
Click here for Hijama Points on the front of the bodyClick here for Hijama Points on the back of the body
Click here for Hijama Points on the head and face
If the client has a complicated history and numerous concerns then it is a good idea to use our online consultation service – click here.
Which body part or function is involved in Neuritis?
The function of all body systems is controlled by the central nervous system (CNS) consisting of the brain and the spinal cord and peripheral nervous system (PNS) consisting of all the nerves that branch outside the central nervous system and spread throughout the body parts. These systems are well-organized to perform the crucial function of how the information is processed and communicated in the body. The adult brain is divided into four main regions including the cerebellum, cerebrum, brain stem, and diencephalon. The neural activity in the brain controls a person’s conscious practices while sensory and motor pathways of the spinal cord control the coordination of the reflexes. The homeostasis of these intricate functions is regulated by the specialized brain area. The main role of the peripheral nervous system is to connect the skin, organs and limbs to the central nervous system by sending and receiving the information to and from the CNS that makes our body react according to the outer environmental stimuli. The nerves of PNS are the bundles of axons and axons from the neurons. The peripheral nervous system is divided into somatic and autonomic nervous systems.
Somatic nervous system
This part of the peripheral nervous system transports the sensory and motor information to and from the CNS. There are two main types of neurons in the somatic nervous system:
Motor neurons
They carry information from the central nervous system to muscle fibers present in the body allowing us to take actions physically to the environmental signals. These are also called efferent neurons based on their activity.
Sensory neurons
Sensory neurons take the information from the body towards the central nervous system and allow humans to receive the sensory information from outside to the brain these are also called afferent neurons.
Autonomic nervous system – This part of the peripheral nervous system regulates the involuntary body functions that include the heartbeat, breathing, blood flow, and digestion.
What are the symptoms and effects of Neuritis on the body?

Neuritis can be described as an inflammation of a nerve or the general inflammation of the peripheral nervous system. Inflammation and frequently concomitant demyelination cause impaired conduction of neural signals and leads to aberrant nerve function. Neuritis is often used interchangeably with the term neuropathy. Neuropathy is usually a painful condition linked with inflammation and nerve damage, dysfunction, or degeneration. Neuritis is either a result of local iron deposition or it may result from the complication of diabetes mellitus (DM) that accompanies most hemochromatosis cases in certain cases, neuritis can proceed to neuropathy.
Mononeuritis
Neuritis affecting only one nerve referred to as mononeuritis, while it may be a plexus of nerves (plexitis). If various single nerves are affected collectively and simultaneously, then this condition is referred to as mono neuritis multiplex.
Polyneuritis
When widely spread nerves are damaged then this condition is known as polyneuritis.
Sensations of tingling, burning or stabbing pains are caused by the inflammation of sensory neurons in the nerve fiber. These sensations are often worse at night and increases in irritation by temperature or touch changes.
While the inflammation of motor neurons results in symptoms that may range from muscle weakness to complete paralysis. The affected nerve may cause muscle tenderness, loss of muscle tone and may lead to atrophy. The Inflammation of a facial nerve, a type of mononeuritis, results in Bell palsy which is the characteristic distortion of the muscles on one side of the face. It is often limited to the caudal spinal nerves and spinal nerve roots.
Brachial Neuritis
The peripheral neuropathy that affects the shoulder, chest, arm, and hand is referred to as brachial neuritis.
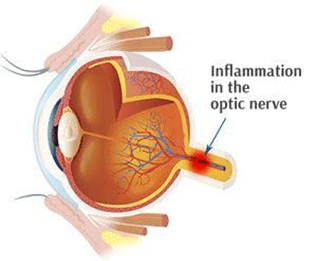
Optic neuritis
It is one of the most common types of neuritis. The most common pathologic basis for optic neuritis is the inflammatory demyelination of the optic nerve. The pathology alike multiple acute sclerosis (MS) plaques in the brain, with perivascular cuffing, myelin breakdown, and edema in the myelinated nerve sheaths. Several autoimmune conditions are usually associated with optic neuritis.
Multiple sclerosis
In multiple sclerosis autoimmune system attacks the myelin sheath which covers the nerve fibers in the brain. In people with optic neuritis, after one episode of optic neuritis the risk to develop multiple sclerosis is about 50% over a lifetime.
Neuromyelitis Optica
It occurs when the inflammation affects the spinal cord and optic nerve and shows some similarity to multiple sclerosis, but it doesn’t cause damage to the nerves in the brain as often as multiple sclerosis does. Yet, it is more severe than MS, usually results in a diminished recovery after an attack as compared to MS.
Myelin oligodendrocyte glycoprotein (MOG) antibody disorder
It can cause inflammation to the spinal cord, optic nerve, or brain. Like neuromyelitis optica and MS, recurrent attacks of inflammation may occur. Recovery from MOG attacks is often better than neuromyelitis optica.
Symptoms might include:
- Pain: Most people who develop optic neuritis experience eye pain which gets worsened during eye movement. At times the pain feels like a dull ache behind the eye.
- Loss of vision: Optic neuritis may result in loss of vision in one eye. Although most people experience at least some temporary reduction in vision the extent of loss varies. Loss of vision is considered noticeable if the duration of loss spans over hours or days, and takes several weeks to a month to get better. Vision loss can be permanent in some people.
- Visual field loss: Loss of side occurring in any pattern, like peripheral vision loss or central vision loss
- Loss of color vision: Optic neuritis usually affects color perception. People may experience that colors appearing less vivid than normal.
- Flashing lights: Sometimes people with optic neuritis report experiencing flashing or flickering lights with eye movements.
What changes in diet can help improve symptoms of Neuritis?
Caregivers should focus on incorporating foods with anti-inflammatory properties into a balanced diet. These foods include whole grains, lean meats, vegetables, nuts, and fish. Lean meats such as poultry and fish are high in vitamin B12, keeping blood cells and nerves healthy.
Changes in lifestyle which can help Neuritis
- Do exercise regularly. Regular exercise may help to alleviate pain or cramps, improve muscle strength, help regulate blood sugar levels, and prevent muscle loss.
- Eat healthily
- Give up Excess Alcohol.
- Manage Diabetes.
Possible alternative remedies for Neuritis
1. Vitamins
Deficiency of certain vitamins leads to neuritis. Vitamin B is essential for nerve health and its deficiency may result in significant nerve damage. Vitamin B can be obtained from food and can also be obtained from supplements as well. Prescribed dosage should be followed to avoid toxicity. Apart from vitamin B, vitamin D deficiency also plays role in peripheral neuropathy. Vitamin D supplements may help to alleviate the symptoms of neuropathy.
2.Cayenne pepper
It contains capsaicin, an ingredient that is responsible for the hotness of spice. It has been used include in a topical cream to relieve the sensation of pain. Capsaicin supplement or incorporating cayenne pepper in diet can help with neuropathy pain. Moreover, topical capsaicin ointments can be applied to the body, although it gives a burning sensation in the beginning gradually reduce the sensation of neuropathy.
3. Quit smoking
Smoking affects blood circulation. It narrows the blood vessels and less oxygenated blood can get through. Improper blood circulation results in the increased numbness and pain due to neuropathy.