Complete Hijama Treatment Plan for Involuntary Urination
Allow 2-4 weeks between sessions – longer if required. Hijama Points shown for each session should ONLY be used to guide the therapist. Body size, cup size, and any other conditions need to considered and appropriate care and attention taken. The number of sessions shown can be increased or reduced depending on the condition of the client.
Complete Treatment Plan
Click here for Session 1Click here for Session 2
Click here for Session 3
Use the standard hijama points as an additional or as separate standalone sessions.
Standard Dry Points – 137,138,139,140,142
Click here for Hijama Points on the front of the bodyIf the client has a complicated history and numerous concerns then it is a good idea to use our online consultation service – click here.
Which body part or function is involved in Involuntary Urination?
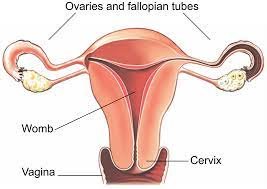
The Lower Urinary Tract (LUT) comprises the urinary bladder, urethral sphincter, and urethra. It serves double functions, storage and excretion of urine. Most of the time LUT performs its major function of storage of fluid coming from the kidneys without letting us pass the urine all the time or incontinently.
Three important features allow LUT to perform this storage function. Firstly, the bladder must be capable of accommodating a large volume of urine which is made possible by the elastic nature of the bladder. The bladder wall is composed of smooth muscle, the detrusor, having the capability to induce constant low tension over a wide range of pressure exerted by the increasing volume of urine. Secondly, the integrity of the peripheral and central nervous system inhibits the premature contraction of smooth muscles during the high-pressure buildup due to urine filling. Lastly, the closed outlet of the bladder, the internal urethral Sphincters (IUS) requires to maintain the high pressure while the external urethral sphincters (EUS) apply tonic tension having the capability for involuntary contraction at the time of need. The combination of the intact, compliant, and relaxed bladder with low pressure during filling and high pressure at IUS and EUS leads to a pressure gradient that allows the storage of urine without involuntary elimination.
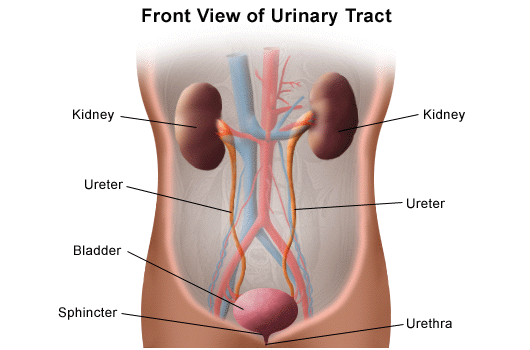
The central nervous system mediates the coordination to make the person aware when to void voluntarily. To allow this, central inhibition of excretion reflex is lifted by inducing contraction of detrusor, ceasing the tonic contraction of EUS and pressure at the bladder neck (IUS) which results in the decrease of outlet pressure, starting the change in pressure gradient and voidance of urine. When the capability of LUT is compromised to perform these functions, it results in crippling functional disorders such as Urinary Incontinence (UI) or involuntary urination, defined as “the complaint of involuntary loss of urine”. This stigmatizing condition has often devastating effects on millions of people around the world.
What are the symptoms and effects of Involuntary Urination on the body?
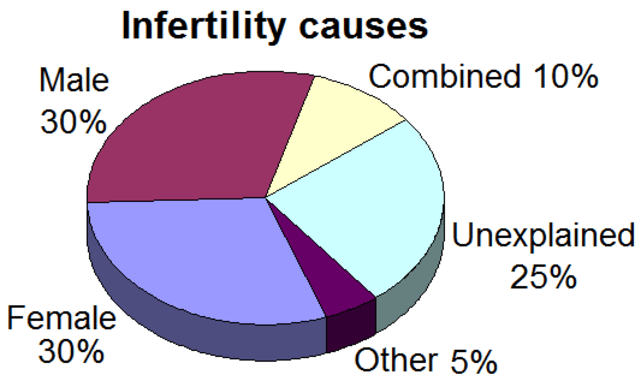
UI is more common in women than men (2:1 ratio), it is often too humiliating for a person with this condition to discuss, so its true prevalence is difficult to determine. Symptoms include bed-wetting, leakage of urine without any urge or feel, a sudden strong urge to urinate, leakage of urine during normal activities like bending, lifting, exercising, and coughing. Causes of temporary UI include constipation, UTI, and the use of certain medicines. UI can be chronic, its causes include weak pelvic floor muscles, overactive bladder muscles, and neurological disorders such as Parkinson’s, multiple sclerosis and stroke, chronic bladder inflammation (interstitial cystitis), obstruction. Some causes are gender-specific such as pregnancy, hysterectomy, menopause, and childbirth in women, and enlarged bladder, prostate cancer, and benign prostatic hyperplasia (BPH) in men. There are many types of UI with stress UI and urge Incontinence is the most common.
1. Stress Incontinence:
It is caused by sudden leakage of urine by sudden contractions or pressure on bladder muscles. It usually occurs during coughing, laughing, heavy weight lifting, exercising, and sneezing. It is the most common bladder problem in young and middle-aged women, in young women, it is caused due to inherent pelvic muscle weakness and stress caused by childbirth. In middle-aged women stress of menopause lead to this condition.
2. Urge Incontinence:
Alternatively called an overactive bladder, it occurs when a person feels a strong urge to urinate but unable to hold back until he reaches the toilet. It occurs after chronic conditions such as Parkinson’s, Alzheimer’s, multiple sclerosis, and stroke and in some cases, it is indicative of bladder cancer.
3. Overflow Incontinence:
it happens when a person is not able to evacuate the bladder completely resulting in an overflow of the bladder as the new urine is entered. It is usually found in persons with spinal cord injuries and diabetes.
4. Functional Incontinence:
This type of incontinence is not related to the problems in the bladder. It mostly occurs in disabled and elderly persons who have normal bladder but find it difficult to move and go to urinate in time due to mobility issues. Nocturnal Incontinence: It is usually found in women and men over the age of 60 years. It is the need to urinate two or more times during the night. In men, it can be a sign of prostate cancer. Mixed Incontinence: It happens when a person experiences symptoms of more than one type of incontinence.
What changes in diet can help improve symptoms of Involuntary Urination?

Key dietary habits or adaptations that help the person to overcome the symptoms and manage UI include balance water intake and avoidance of certain food. Water intake should be balanced as too much water will cause burdened the bladder and a lower quantity will cause concentrated urine leading to bladder inflammation. Following food items should be avoided to cope with UI symptoms.
- Alcohol: as it directly affects the bladder by interfering with the CNS control over the urination control and evacuation.
- Caffeinated drinks and foodstuff: as it irritates the bladder lining. Spicy food should be cut off especially if a person has an overactive bladder.
- Spicy foods: like caffeine, spicy foods also cause bladder lining inflammation.
- Citrus fruits and carbonated drinks:They should be cut off as acid in citrus fruits and carbon dioxide in carbonated drinks increase bladder irritation.
Changes in lifestyle which can help Involuntary Urination
Certain lifestyle changes can help to reduce the symptoms of UI. Pelvic floor exercises should be done regularly because they are effective in reducing leakage. Smoking causes coughing which puts stress on pelvic muscles so it should be avoided. If the person is obese he must lose extra weight as fat around the bladder increases pressure. Moreover, collectors and pads could be used to avoid leakage or to handle smaller amounts of urine like sanitary napkins or protective undergarments with high-tech lining which will prevent the liquid to break down the skin.
Possible alternative remedies for Involuntary Urination
There is evidence of the effectiveness of conventional and alternative medicines for urinary incontinence. Mind-body interventions such as pelvic floor muscle training, yoga, and bladder muscle training, a manipulative body-based approach like massage, energy therapy, and use of herbal medicines like corn silk, capsaicin, Ganoderma Lucidum, and Gosha-jinki-gan (blend of 10 Chinese herbal medicines) are effective alternative ways to cope with UI.